Acute Renal Failure
Acute kidney injury (AKI)
requiring renal replacement therapy (RRT) in critically ill patients results in
a high hospital mortality. Outcome prediction in this selected high-risk
collective is challenging due to the lack of appropriate biomarkers. The aim of
this study was to identify outcome-specific biomarkers in this patient
population.
METHODS: Serum samples
were collected from 101 critically ill patients with AKI at the initiation of
RRT in intensive care units (ICUs) of tertiary care university hospital between
August 2008 and March 2011. Measurements of serum levels of cystatin (CysC),
neutrophil gelatinase-associated lipocalin, and interleukin-18 (IL-18) were
performed. The primary outcome measure was hospital mortality.
RESULTS: The observed
overall mortality rate was 56.4% (57/101). Multiple logistic regression analysis
indicated that the serum IL-18 and CysC concentrations and Acute Physiology and
Chronic Health Evaluation III (ACPACHE III) scores determined on the first day
of RRT were independent predictors of in-hospital mortality. The APACHE III
score had the best discriminatory power (0.872 ± 0.041, p < 0.001), whereas
serum IL-18 had the best Youden index (0.65) and the highest correctness of
prediction (83%). Cumulative survival rates at 6-month follow-up following
hospital discharge differed significantly (p < 0.001) for serum IL-18 <1786 ng/ml
vs. ≥1786 pg/ml in these critically ill patients.
CONCLUSION: In this
study, we confirmed the grave prognosis for critically ill patients at the
commencement of RRT and found a strong correlation between serum IL-18 and the
hospital mortality of ICU patients with dialysis-dependent AKI. In addition, we
demonstrated that the APACHE III score has the best discriminative power for
predicting hospital mortality in these critically ill patients.
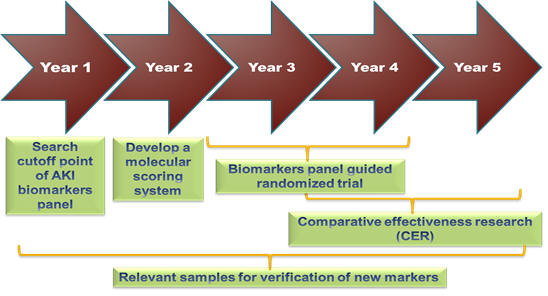
AKI biosignature Plan